AI Breakthrough: Cleveland Clinic and IBM Unveil Non-Opioid Pain Management Solutions
A team of scientists at Cleveland Clinic has teamed up with IBM, and they're cooking up something big in the world of medicine. These folks aren't just playing around in the lab - they're using some seriously smart computer tech to tackle a problem that's been giving doctors headaches for years.
Dr. Feixiong Cheng is leading the charge, and his team is diving into a sea of data that would make most of us dizzy. They're not after a run-of-the-mill discovery, though. Nope, they're aiming for a game-changer that could help millions of people.
What exactly are they up to? Well, that's the million-dollar question. But one thing's for sure - if they pull this off, it could flip the script on how we think about keeping people healthy.
The Chronic Pain Crisis

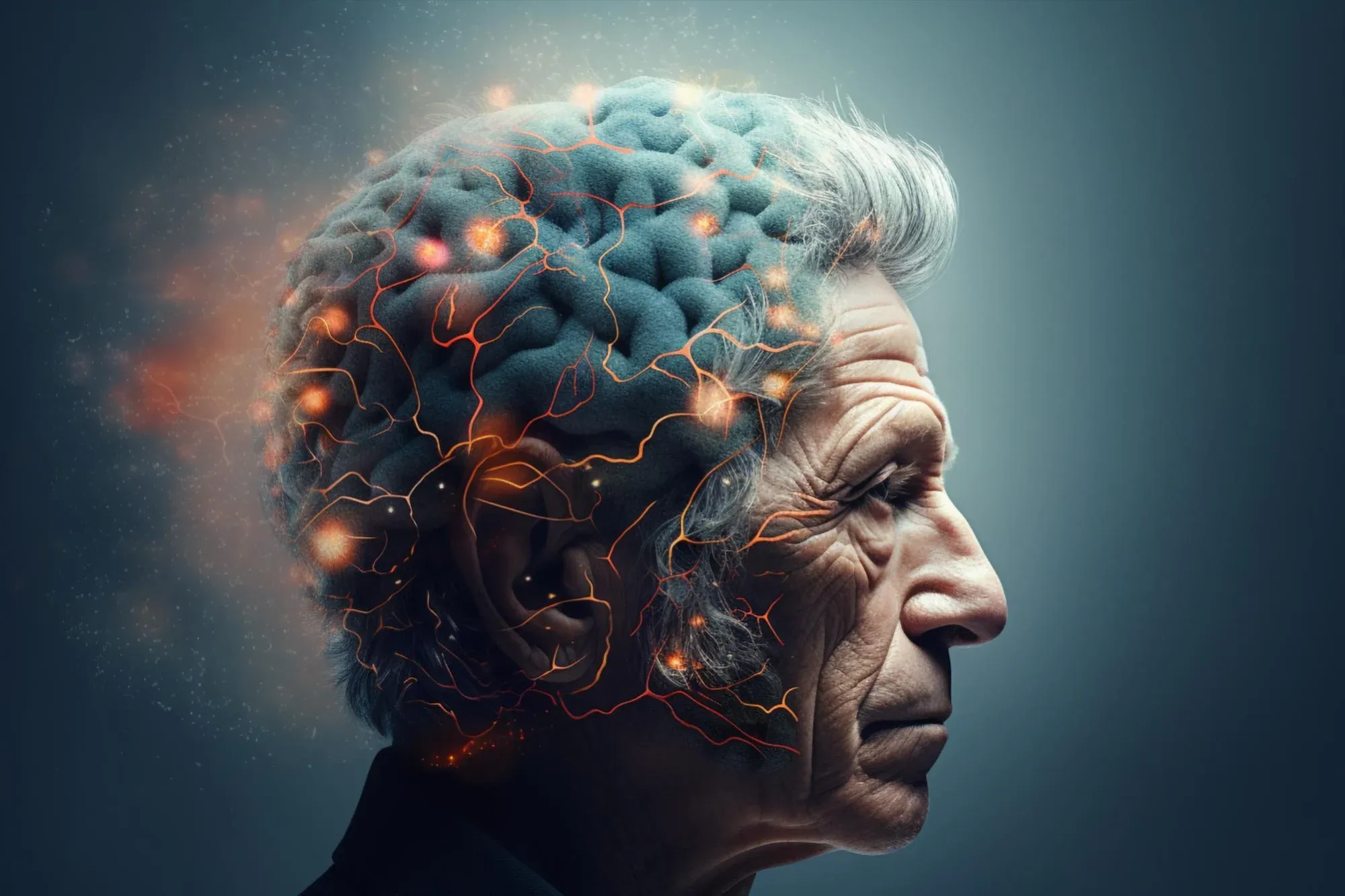
Image Credit: UT news
Chronic pain affects millions of Americans, causing ongoing suffering and reducing quality of life. Recent studies show that about 1 in 5 U.S. adults deal with chronic pain. This means over 50 million people live with pain that lasts for months or even years.
The impact of chronic pain goes beyond physical discomfort:
It often leads to mental health issues like depression and anxiety
Many people with chronic pain struggle to work full-time
Everyday activities like household chores become challenging
Sleep problems are common, further affecting overall health
Current treatments for chronic pain have major drawbacks. Over-the-counter painkillers may not be strong enough for severe pain. Physical therapy and alternative treatments can help some people but don't work for everyone.
Opioids are very effective at reducing pain, which is why doctors often prescribe them. However, opioids come with serious risks:
They can be highly addictive
It can increase the risk of cardiovascular events
Overdoses are possible, especially with long-term use
Side effects like constipation, drowsiness, and hormonal imbalances are common.
This creates a difficult situation. Opioids work well for pain relief, but the potential for addiction and other problems is high. Many people with chronic pain feel stuck between living with constant pain or risking opioid-related issues.
Finding new ways to manage chronic pain without relying on opioids has become a top priority in healthcare. The search for effective, non-addictive treatments continues as the chronic pain crisis affects more and more Americans.
Cleveland Clinic and IBM: A Powerful Partnership

The fight against chronic pain has gained a powerful ally in the form of a partnership between Cleveland Clinic and IBM. This collaboration, known as the Discovery Accelerator, brings together medical expertise and cutting-edge technology to tackle some of healthcare's biggest challenges.
At the heart of this partnership is Dr. Feixiong Cheng, the Director of Cleveland Clinic's Genome Center. Dr. Cheng leads a team of talented researchers, including:
Dr. Yunguang Qiu, a postdoctoral fellow specialising in nervous system disorders
Dr. Yuxin Yang, a computational scientist and data expert
These researchers are working hand-in-hand with IBM's technology experts to push the boundaries of medical research.
IBM's role in this partnership is crucial. They bring:
Advanced artificial intelligence capabilities
Powerful computing resources
Industry expertise in developing new technologies
The team is using AI to speed up the drug discovery process for pain management. Their approach looks at existing FDA-approved drugs and natural compounds from the gut to find new ways to treat pain without opioids. This method could save years of research time and millions of dollars in development costs.
The Discovery Accelerator partnership is just getting started, but it's already showing promise in the field of pain management. As this collaboration continues, it could pave the way for new treatments and a better understanding of chronic pain.
The AI Approach to Pain Management

Scientists are taking a new approach to pain management, using artificial intelligence to find better treatments. This method focuses on special proteins in our bodies called G protein-coupled receptors, or GPCRs for short.
GPCRs play a big role in how we feel pain:
They act like tiny switches in our cells
Some GPCRs can turn pain signals on or off
Targeting specific GPCRs could help manage pain without addiction risks
Instead of creating new drugs from scratch,researchers are looking at medicines we already have. This idea is called drug repurposing. It's like finding a new use for a tool you already own.
Drug repurposing has some big benefits:
It's faster than developing new drugs
We already know these drugs are safe for people
It can be less expensive than traditional drug development
To make this process even faster, Dr. Cheng's team created a special AI tool called LISA-CPI. This tool is can find potential pain treatments.
Here's what LISA-CPI does:
It looks at thousands of existing drugs and natural compounds
It predicts how these compounds might interact with pain receptors
It helps researchers focus on the most promising options
The LISA-CPI tool uses deep learning, a type of AI that can spot patterns humans might miss. It can quickly sort through huge amounts of data about drugs and proteins.
How LISA-CPI Works

LISA-CPI(Ligand Image- and receptor's three-dimensional (3D) Structures-Aware framework to predict Compound-Protein Interactions) is a powerful AI tool that's changing how we look for new pain treatments. It's like having a super-smart scientist that can work incredibly fast. Let's break down what this AI can do:
LISA-CPI has some amazing abilities:
It can predict if a drug will attach to a pain receptor
It figures out where exactly the drug will stick to the receptor
The AI can tell how strongly the drug will bind
It even predicts if the drug will turn the pain signal on or off
To do all this, LISA-CPI needs to understand molecules in 3D.
This is really important because:
Drugs work by fitting into receptors like a key in a lock
The shape of both the drug and the receptor matters a lot
Small changes in shape can make a big difference in how drugs work
Creating these 3D models used to take a long time. Scientists had to piece together lots of information about each molecule's structure and properties. But LISA-CPI can do this much faster.
Here's how AI speeds up the process:
It can look at thousands of molecules at once
The AI learns from every bit of data it sees
It combines information from many different experiments
In one study, LISA-CPI looked at:
369 natural compounds from gut bacteria
2,308 drugs already approved by the FDA
How these might interact with 13 different pain receptors
This would take humans years to do, but the AI did it quickly. The best part is that LISA-CPI doesn't just work faster - it can spot things humans might miss.
Discovery Accelerator Methodology and Findings

The team at Cleveland Clinic and IBM recently shared their exciting work in a well-known science journal called Cell Press. This study shows how AI can help find new ways to treat pain. Let's look at what they did and what they found.
The researchers used their LISA-CPI tool to look at a lot of different compounds:
369 natural substances made by gut bacteria
2,308 drugs already approved by the FDA
13 different pain receptors in the body
That's a total of 2,677 compounds checked against 13 receptors - a huge task that would take humans a very long time to do.
Here's how they did it:
They fed information about these compounds into LISA-CPI
The AI predicted how each compound might interact with the pain receptors
It looked for compounds that could attach to receptors in helpful ways
The results were promising:
The AI found several compounds that might work as pain treatments
Some of these were existing drugs that could be used in new ways
Others were natural substances made by the bacteria in our gut
The team isn't stopping here. They're now testing these compounds in the lab to see if they really do work as pain treatments. This is an important next step to make sure the AI's predictions are right.
Future Applications of LISA-CPI
The success of LISA-CPI in finding potential pain treatments is just the beginning. This AI tool has exciting possibilities for tackling other health problems too.
Dr. Yang and his team are thinking big:
They want to use LISA-CPI to look for Alzheimer's treatments
The AI could help with other brain diseases as well
The team is also working on something called "small molecule foundation models." These are like building blocks that can help create new drugs.
They're using AI to:
Understand how tiny molecules work in our bodies
Find new ways these molecules could be used as medicine
Right now, there's an ongoing project to discover completely new drugs. This is different from repurposing existing ones. It's more challenging, but it could lead to big breakthroughs.
The researchers believe AI tools like LISA-CPI will:
Speed up the process of finding new treatments
Help solve tough health problems we haven't cracked yet
Make drug discovery faster and less expensive
While there's still a lot of work ahead, these AI tools are giving scientists new ways to fight disease and improve health for everyone.
Conclusion
Cleveland Clinic and IBM have joined forces to revolutionize pain management using artificial intelligence. Their Discovery Accelerator partnership, led by Dr. Feixiong Cheng, aims to address the chronic pain crisis affecting one in five Americans.
The team developed LISA-CPI, an AI tool that rapidly analyzes existing FDA-approved drugs and gut microbiome metabolites to identify potential non-opioid pain treatments.
This innovative approach targets specific G protein-coupled receptors (GPCRs) associated with pain, potentially offering safer alternatives to addictive opioids.
The AI examined 2,677 compounds against 13 pain receptors, uncovering promising candidates for further testing. Beyond pain management, LISA-CPI shows potential for accelerating drug discovery in other areas, such as Alzheimer's treatment.
While the journey from AI-discovered drugs to market approval remains lengthy, this breakthrough represents a significant step forward in leveraging technology to combat chronic pain and reduce opioid dependence.
FAQs
1. How long does it typically take for an AI-discovered drug to reach the market?
AI-discovered drugs still need to go through lab testing, animal trials, and human clinical trials. This process can take 5-10 years or more. While AI speeds up the initial discovery, the safety testing and approval process still takes a long time.
2. Are there any risks associated with AI-driven drug discovery?
AI might miss important factors that humans would notice, leading to overlooked side effects. There's also a risk of bias in the data AI uses, which could affect results. However, these risks are generally lower than traditional drug discovery methods.
3. What role does the gut microbiome play in pain management?
The gut microbiome produces natural compounds that can affect pain. Some of these might work like pain relievers. AI tools like LISA-CPI are looking at these gut-made substances to find new ways to manage pain without using addictive drugs.
Comments
Your comment has been submitted